By Laura Pinsoneault, Kelly Hacket, Tobi Cawthra
The quality of a mammogram may be about more than the routine technical aspects of completing the breast scan at a clinic. At least that’s what patients are telling us in interviews conducted by the Mammographic Quality Initiative (MQI), a project of the Community and Cancer Science Network (CCSN).
Differences in breast cancer mortality exist for many reasons, including biological, individual, and social reasons. Uncovering the many factors which may influence mammography quality could help us understand why some patients have different breast cancer outcomes. For example, Black women have higher breast cancer mortality rates despite having similar mammography screening rates as women of other races and ethnicities. We also see higher mortality in certain regions of Wisconsin.
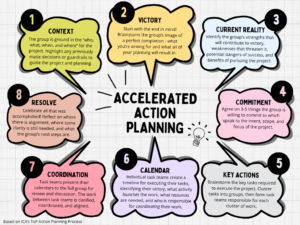
The MQI project is working to understand the factors that contribute to quality, in part, by asking women about how they define a quality mammogram. The insights generated through these interviews will inform how to improve measures of quality and create a statewide, shared measurement system to monitor and improve quality and promote equity of early-stage breast cancer diagnosis. And this includes survival rates.
While the professionals who perform mammograms may emphasize the technical aspects a mammogram when assessing the quality of the exam, patients care about other measures. Of course, patients highly value the imaging, interpretation and follow-up after the exam but they also consider such factors as availability of the procedure, transportation and the hours of operation in their overall quality assessment. They also have other concerns. How well do the providers communicate? Does gender, race or class-based bias exist? Do patients feel safe and cared for? How can we make mammograms physically and psychologically more comfortable?
The initial findings from interviews with women accessing mammograms indicate that the current measures alone may not adequately define quality. This may indeed be an important explanation for why disparities exist when it comes to mammography in Wisconsin.
Elevating patient perspectives in defining quality may offer significant opportunities to change the way mammograms are performed from a systems perspective. In doing so, we could improve the overall quality of this exam, better serving the very patients who depend on a mammogram to safeguard their good health.
Making progress in this regard, may help us figure out how to eliminate or at least lessen the disparities that lead to premature death in Wisconsin.
Laura Pinsoneault, PhD, is President and CEO of Evaluation Plus.
Kelly Hacket, MPH is the MQI Project Manager at Wisconsin Women’s Health Foundation
Tobi Cawthra, MPH is the Program Director of the Community & Cancer Science Network based at the Medical College of Wisconsin.